There is broad acceptance in the scientific, medical, and financial communities that chronic inflammation is a significant factor in many chronic diseases, particularly cardiovascular disease. The double-blind, randomized, placebo-controlled CANTOS clinical trial (10,061 patients; Novartis, 2017) and REDUCE-IT clinical trial (8,179 patients; Amarin Corporation, 2018), both published in the New England Journal of Medicine, helped to catalyze and support this consensus. Commonly used anti-inflammatory drugs such as aspirin, ibuprofen, naproxen, COX-2 inhibitors, corticosteroids, and various biologics may reduce inflammation, but they have risks of significant side effects that limit their utility in chronic disease.

We believe that a safe anti-inflammatory is the solution. Our lead pharmaceutical candidate CDX-101, a proprietary prodrug of the naturally occurring marine molecule astaxanthin, may provide the needed combination of an excellent safety profile, anti-inflammatory activity, and economic pricing to become widely used for the prevention and treatment of chronic diseases driven by inflammation.
We are pursuing an initial indication of severe hypertriglyceridemia (“SHTG”) (triglycerides ≥ 500 mg/dL) for CDX-101. Severe hypertriglyceridemia is associated with chronic inflammation and patients with the disorder have increased cardiovascular disease risk and incidence of pancreatitis. We believe the clinical pathway to U.S. Food and Drug Administration (“FDA”) drug approval for severe hypertriglyceridemia, which relies on biomarker endpoints (i.e., measuring triglycerides in blood tests over a period of several months), will be more efficient than other potential indications that require clinical outcomes studies (e.g., evaluating heart attacks, strokes, and deaths over a period of several years), and is thus better suited as our initial indication for CDX-101.
About Severe Hypertriglyceridemia
An estimated 3.4 million Americans have severe hypertriglyceridemia according to peer-reviewed research published in the American Journal of Cardiology in 2011. Statins, fibrates, and prescription fish oils are all used to manage hypertriglyceridemia. 21% (42 million) of U.S. adults have mixed dyslipidemia (high levels of low-density lipoprotein “LDL” cholesterol with low levels of high-density lipoprotein “HDL” cholesterol and/or high levels of triglycerides), with nearly 6% (11.6 million people) having all three lipid abnormalities. Lovaza, Vascepa, and other prescription fish oils approved for severe hypertriglyceridemia are also used off-label in mixed dyslipidemia patients to reduce moderately elevated triglycerides and aggregate sales of these products for on and off-label use are estimated to be approaching $2 billion annually.
3400000
An estimated 3.4 million Americans have severe hypertriglyceridemia.
There are multiple etiologies of severe hypertriglyceridemia. In general, disease pathogenesis can be broken down into acquired vs. inherited disorders. According to a recent population-wide study in the U.S., acquired conditions most strongly associated with severe hypertriglyceridemia include type II diabetes, elevated cholesterol, and chronic renal disease (Christian, Am J Cardiol, 2011). Additionally, almost 90% of individuals with severe hypertriglyceridemia were either overweight or obese, and they tended to be older, Caucasian men. Meanwhile, several inherited defects in lipid metabolism can lead to severe hypertriglyceridemia, including Chylomicronemia Syndrome, Familial Combined Hyperlipidemia, and Hyperbetalipoproteinemia. These disorders present much earlier in life with additional skin findings, such as xanthomas, and are significantly less common (Miller, Circulation, 2011).
While elevated serum triglycerides can be largely asymptomatic, several genetic and epidemiologic studies have implicated elevated serum triglycerides as an independent risk factor for the development of atherosclerotic cardiovascular disease and subsequent CV events (Faergeman, Am J Cardiol, 2009; Miller, J Am Coll Cardiol, 2008; Freiberg, JAMA, 2008). Atherosclerotic plaques arise when lipids enter the intimal layer of a blood vessel and become oxidized. Macrophages then ingest these oxidized lipids to become foam cells, which can release a wide array of chemokines, cytokines, and reactive oxygen species (ROS). These signaling molecules stimulate smooth muscle migration, collagen deposition, and ultimately thickening of the vessel wall (Ruparelia, Nat Rev Cardiol, 2017; Hansson, NEJM, 2005). Chronic inflammation serves to maintain and propagate atherosclerotic changes (Ruparelia, Nat Rev Cardiol, 2017; Hansson, NEJM, 2005). Ruptured plaques can stimulate clot formation within the affected vessel. This may manifest as a heart attack or stroke if the coronary or cranial vasculature is affected, respectively.
Elevated serum triglycerides are thought to contribute to plaque development in several ways. Triglycerides are shuttled throughout the vasculature on molecules called lipoproteins, which consist of varying ratios of proteins, cholesterol, and triglycerides. Triglyceride-rich lipoproteins (TGRLs) are thought to be particularly pathogenic (Nordestgaard, Lancet, 2014). TGRLs can enter and are retained within the intimal layer of the vessel, thereby directly increasing lipid deposition and subsequent oxidation. Additionally, TGRLs can activate a number of pro-inflammatory pathways implicated in plaque development, including endothelial cell activation and apoptosis as well as macrophage and neutrophil recruitment (Wang, PLoS One, 2013; Aung, Arterioscler Thromb Vasc Biol, 2013; Toth, Vasc Health Risk Manag, 2016). TGRLs are also pro-thrombogenic, enhancing platelet aggregation and clot formation (Olufadi, Pathophysiol Haemost Thromb, 2006; Toth, Vasc Health Risk Manag, 2016). It is clear that elevated triglycerides, and TGLRs in particular, can greatly influence the development of atherosclerosis and downstream consequences.
First-line therapy for severe hypertriglyceridemia is typically a high-intensity statin. In addition to lowering LDL cholesterol, statins can also substantially reduce serum triglycerides (Hunninghake, Coron Art Dis, 2004; Bakker-Arkema, JAMA, 1996). In individuals with persistently elevated serum triglycerides or in those who cannot tolerate statin therapy, there are currently three approved pharmacologic interventions specifically for lowering serum triglycerides: fish oil, fibrates, and niacin.
These agents are meant to complement lifestyle modifications, such as diet and exercise. Although each therapy can substantially reduce triglyceride levels, only fish oil has shown direct clinical benefit in reducing CV risk. More specifically, the REDUCE-IT trial recently demonstrated that the highly purified fish oil, icosapent ethyl, reduced the combined risk of CV death, MI, stroke, unstable angina, and CV revascularization (Bhatt, NEJM, 2019). However, the benefit to individuals with severe hypertriglyceridemia is still unknown, as the trial excluded those with triglyceride levels >500 mg/dl. No evidence exists to suggest a CV risk reduction with niacin, while evidence for fibrates is derived largely from subgroup analyses in other clinical trials (Manninen, Circulation, 1992; Elam, JAMA Cardiol, 2017).
Each of these agents also comes with a host of unwanted side effects. Fish oil, and particularly icosapent ethyl, can lead to gastrointestinal discomfort, joint pain, and sore throat (Wang, Am J Clin Nutr, 2006). Fibrates can cause muscle toxicity, especially when used with a statin (Pierce, JAMA, 1990). Niacin can also cause severe unwanted skin flushing, itching, and diarrhea (Grundy, Arch Int Med, 2002). With this in mind, it is not surprising that only about 15% of patients with severe hypertriglyceridemia use a lipid-lowering agent, with the vast majority using statin monotherapy over any of the above triglyceride-specific treatments (Christian, Am J Cardiol, 2011). This still leaves a substantial portion of the severe hypertriglyceridemia population without either primary or secondary prevention against CV events. Additionally, even the statin monotherapy group is not free from risk. It was previously shown that elevated serum triglycerides increase risk of recurrent CV events in high risk individuals already on a statin regimen (Faergeman, Am J Cardiol, 2009; Miller, J Am Coll Cardiol, 2008). It therefore stands to reason that these individuals would receive an additional benefit with interventions that directly target serum triglyceride levels.
Astaxanthin and Cardiovascular Health
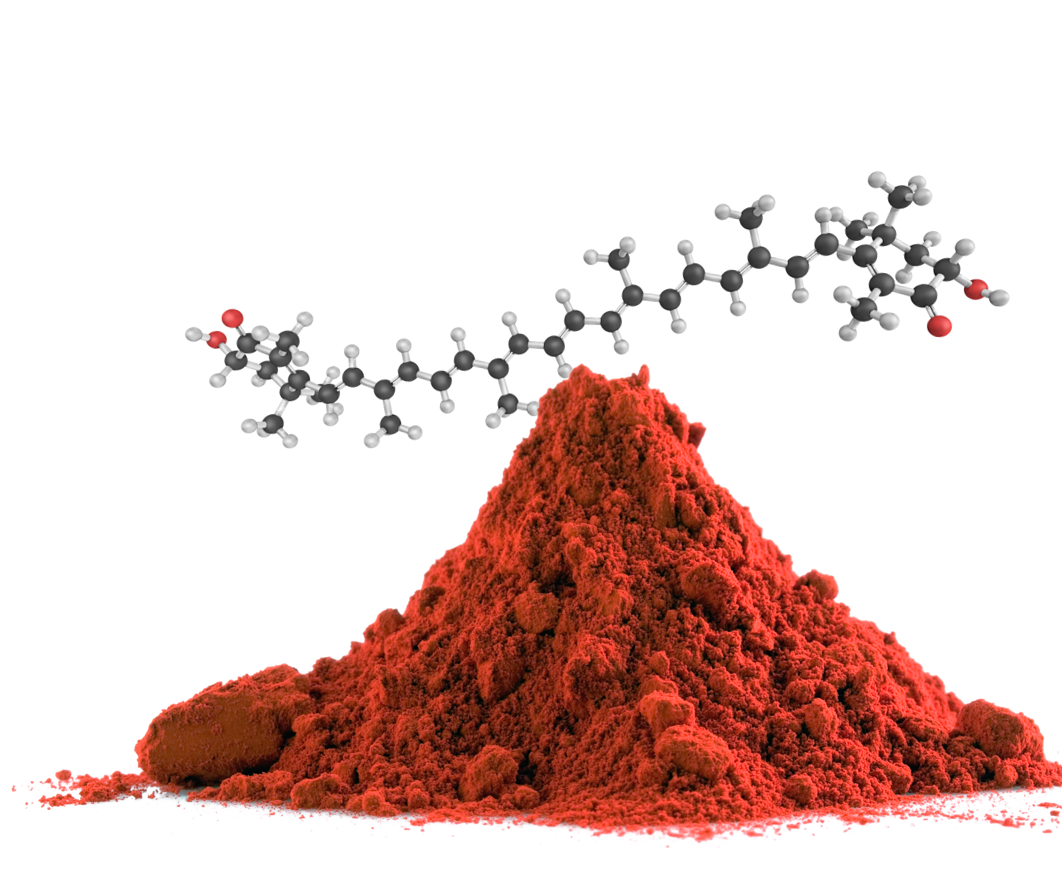
There is a clear clinical need for well-tolerated triglyceride-lowering therapies with beneficial effects on CV disease risk in the severe hypertriglyceridemia population. Astaxanthin, a keto-carotenoid, has emerged as an intriguing therapeutic agent in this population for multiple reasons.
Astaxanthin is a red pigment produced by marine creatures. It is known to have strong anti-oxidant and anti-inflammatory properties that may promote longevity. In the context of metabolic health, not only does astaxanthin lower serum triglycerides, but it also modulates multiple dysfunctional pathways involved in atherosclerosis. For this reason, researchers at Cardax are developing a synthetic astaxanthin compound, CDX-101, for CV risk reduction in patients with severe hypertriglyceridemia.
A growing body of evidence from animal studies and clinical trials suggest that astaxanthin modulates lipid metabolism and CV health in a meaningful way. In different mouse models of CV disease, CDX-085, a pro-drug of astaxanthin previously developed by Cardax, was shown to reduce total serum cholesterol, serum triglycerides, and aortic arch atherosclerosis (Ryu, Atherosclerosis, 2012). CDX-085 also reduced thrombi and increased blood flow in a mouse model of oxidative stress-induced thrombus (Khan, Thromb Res, 2010).
Beyond dysregulated lipid metabolism, it is now well-established that chronic inflammation plays an important role in CV disease (Ridker, Lancet, 2018). Astaxanthin has pronounced anti-oxidant and anti-inflammatory properties that may mitigate this pathologic process. For instance, astaxanthin treatment was shown to reduce lipid peroxidation in the peripheral circulation of healthy adults (Iwamoto, J Atheroscler Thromb, 2000; Karpi, Int J Vitamin Nutr Res, 2007). Lipid peroxidation, as discussed above, is one of the initial steps in plaque formation. Separately, in a cohort of obese and overweight adults, which perhaps more closely approximates severe hypertriglyceridemia patients, astaxanthin supplementation reduced multiple markers of oxidative stress and reduced LDL cholesterol levels after 12 weeks of treatment (Choi, Phytother Res, 2011; Choi, Plant Foods for Human Nutrition, 2011).
Potential Advantages of CDX-101
All individuals with severe hypertriglyceridemia are at increased risk for CV events, yet the vast majority are not utilizing available pharmacologic interventions as primary or secondary prevention. This speaks to the opportunity for novel, more effective and tolerable therapies to provide better preventative healthcare to a large number of patients.
We believe CDX-101 will have several competitive advantages compared to prescription fish oils: (i) ease of administration: oral dosing of large fish oil capsules is problematic, whereas we expect CDX-101 tablets should be far smaller; (ii) scalability: prescription fish oil manufacturing is limited by the declining global fish supply, whereas we believe the synthetic production of CDX-101 is scalable; and (iii) safety: prescription fish oils have certain safety risks, whereas we believe that astaxanthin, the active moiety of CDX-101, has an excellent safety profile.
The REDUCE-IT clinical trial demonstrated that administration of Vascepa resulted in a significant reduction of major adverse cardiovascular events (“MACE”) in patients with mixed dyslipidemia on standard of care, specifically statins, and we believe is the primary basis of Amarin’s request to the FDA to expand Vascepa’s label. The reduction of triglycerides in the REDUCE-IT clinical trial was modest however, and the study’s authors concluded that Vascepa’s ability to reduce other markers of cardiovascular disease, including inflammation and oxidized LDL (as demonstrated in the MARINE and ANCHOR clinical trials), provided the pleiotropic effects that led to reduction of MACE in REDUCE-IT. In human proof-of-concept “pilot” studies conducted by third parties and animal models conducted by third parties and us, astaxanthin, the active moiety of CDX-101, has demonstrated similar pleiotropic effects, which are derived from its broad anti-inflammatory activity, but without the limitations of Vascepa or other prescription fish oils. As a result, we believe this market also presents a major opportunity as a potential second indication for CDX-101.
Beyond cardiovascular disease, we believe CDX-101 could be developed to address other chronic diseases driven by inflammation, including metabolic disease, liver disease, arthritis, and aging, each with potential annual sales exceeding a billion dollars.
Cardax may seek to monetize its CDX-101 pharmaceutical assets through licensing or sale.
