CDX-301 is our zeaxanthin pharmaceutical candidate for macular degeneration.
Zeaxanthin has a mechanism of action and excellent safety profile similar to astaxanthin, but it accumulates in the human eye through uptake by a unique retinal receptor, providing protection against blue light, oxidative damage, and related inflammation that occurs in macular degeneration. Pre-clinical and clinical studies with zeaxanthin have demonstrated proof-of-concept for the treatment of macular disorders.
We may seek to monetize our CDX-301 pharmaceutical assets through licensing or sale.
Zeaxanthin and Lower Oxidative Stress
The adult human retina is believed to lack regenerative capacity. Therefore, the RPE cells, which possess significant levels of antioxidants and antioxidant enzymes, are thought to be the key regulators of cellular health of the retina (Cai, Prog Retin Eye Res, 2000; Simó, J Biomed Biotechnol, 2010; Strauss, Physiol Rev, 2005).
These cells are under significant oxidative stress from the toxic byproducts generated in macular degeneration. It is hypothesized that in individuals with macular degeneration, an increased rate of lipofuscin accumulation leads to depletion of the retinal antioxidant defenses. The increased stress and decreased defenses lead to RPE dysfunction, increased RPE cell death, and ultimately contributes to photoreceptor death and loss of vision.
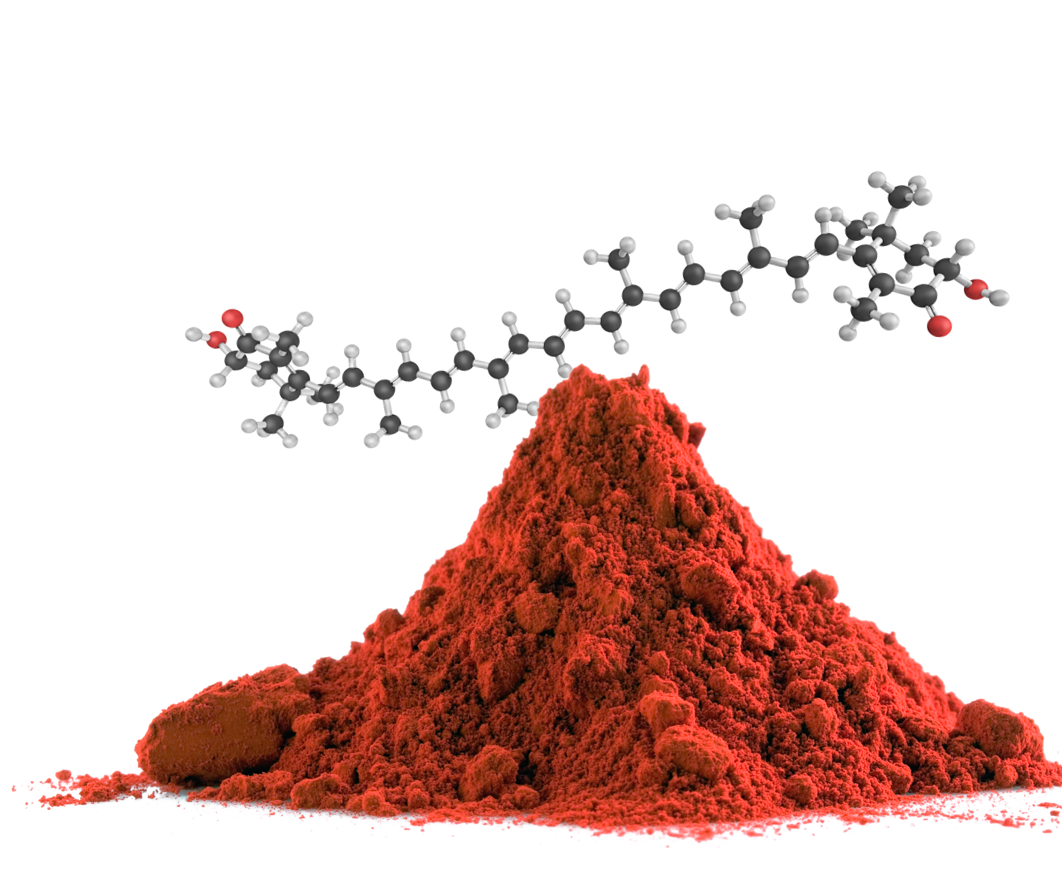
Given that oxidative stress is directly involved in the generation of the toxic byproduct A2E and accelerates visual loss in patients with macular degeneration, researchers at Cardax are currently exploring pharmacologic opportunities to reduce oxidative stress. One promising therapeutic opportunity is zeaxanthin, a xanthophyll carotenoid.
Carotenoids are natural pigments which occur ubiquitously in all organisms capable of conducting photosynthesis and they support animal health and vitality. Although not synthesized by animals, they can be obtained through diet and are present in blood and tissues. Carotenoids are important sources of vitamin A and are known to have strong antioxidant properties. Carotenoids have been shown to have potent anti-inflammatory activity and support mammalian longevity. Research suggests that carotenoids can play a protective role in a number of disorders caused by oxidative stress including cardiovascular disease, certain types of neurological disorders and cancers, and eye-related disorders (Fiedor, Nutrients, 2014).
Zeaxanthin is a carotenoid pigment that protects the macula against blue light and oxidative damage. It is known to preferentially accumulate in the human macula and peripheral retina. Studies have shown a positive relationship between increased zeaxanthin intake and lower oxidative stress (Bernstein, Prog Retin Eye Res, 2016; Kvansakul, Opthalmic Physiol Opt, 2006).
Preclinical Evidence Supporting Zeaxanthin in Macular Degeneration
Zeaxanthin’s protective effects come, in part, from its ability to absorb blue light. Photo receptors are susceptible to damage by light, particularly in the blue visible spectrum. Blue light greatly enhances oxidative stress, the formation A2E, and ultimately the buildup of lipofuscin (Boulton, J Photochem Photobiol B, 1993; Sparrow, Vision Res, 2003). Studies have demonstrated that zeaxanthin is protective, in part, due to its ability to prevent the build-up of the toxic metabolites of Vitamin A after blue-light induced photoreceptor damage (Kim, Exp Eye Res, 2006; Bhosale, Arch Biochem Biophys, 2009). A 2002 in vivo study of quails (animals who similarly have high concentrations of zeaxanthin in the macula), supported this finding by demonstrating that retinal zeaxanthin dose-dependently reduced light photoreceptor apoptosis in the macula (Thomson, Invest Opthalmol Vis Sci, 2002).
Higher levels of macular carotenoids have also been associated with improved outcomes in certain forms of macular degeneration, especially age-related macular degeneration (Kim, Exp Eye Res, 2006; Chew, Opthalmology, 2013).
Some studies have demonstrated an inverse relationship between macular zeaxanthin levels and macular degeneration risk (Zhao, Arch Opthalmol, 2003; Kvansakul, Opthalmic Physiol Opt, 2006). The severity of macular degeneration has been shown to relate to macular pigment depletion in the fovea (Tomas, Invest Ophthalmol Vis Sci, 2009), as patients with higher levels of zeaxanthin are found to have better maintenance of peripheral vision compared to controls.
An in vitro study on the ability of zeaxanthin to protect the RPE cell line against oxidative insults was conducted by Cardax. Using a human retinal-pigmented epithelial line, the researchers assessed the ability of zeaxanthin to protect RPE cells by preparing a control cell line and a cell line incubated with a zeaxanthin formulation (CDX-380). They then challenged these cell lines with different oxidant insults (hydrogen peroxide, 4-HNE, and SIN-1, peroxynitrite). Across the forms of oxidative insult studied, the researchers found decreased cell death in all cell lines pre-treated with CDX-380. They were also able to show that after short-term hydrogen peroxide challenge, zeaxanthin was associated with decreased intracellular signaling in pathways normally activated by oxidative stress. These findings indicate that zeaxanthin is protective against RPE cell death under oxidative stress.
Given that zeaxanthin is associated with lower oxidative stress and improved outcomes in SGTD and findings that dietary supplementation increases serum and macular levels of zeaxanthin (Bone, Exp Eye Res, 2000 ; Hammond, Invest Ophthalmol Vis Sci, 1997; Kvansakul, Opthalmic Physiol Opt, 2006), even in patients with diseased retina (Koh, Exp Eye Res, 2004), it follows that pharmacological supplementation could benefit patients with macular degeneration.
